7/9/2020
Study Aims to Predict the Unpredictable
By John Tibbetts
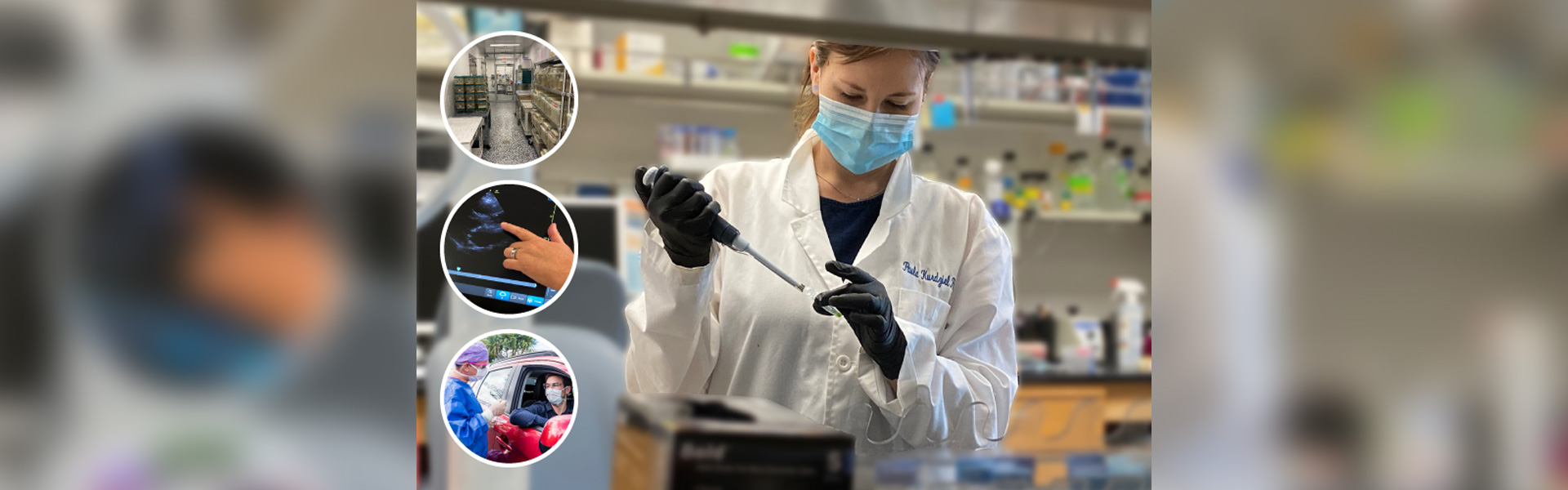
Employers want to keep employees safe from the coronavirus, but testing for COVID-19 is often slow or unavailable. People often don’t know when they’ve been infected, and may show symptoms days later or never show symptoms at all. The great majority of people tested for the presence of COVID-19 already present symptoms, which can lag for days after the infections occur, causing them to unknowingly spread the virus.
In an attempt to reduce this ambiguity, researchers from the Charles E. Schmidt College of Medicine will study 200 randomly chosen residents and faculty volunteers for a period of three months with the goal of developing predictive algorithms of COVID-19 infection.
“We are looking at COVID-19 prevalence in a population of healthcare professionals,” said Massimo Caputi, Ph.D., a professor of biomedical science. “We want to identify when individuals become infected, when or if their bodies react with symptoms, and when their immune systems develop antibodies to the infection.”
Colleagues involved in the study include Janet Robishaw, Ph.D., senior associate dean for research and chair of the Department of Biomedical Science, and Joanne Krasnoff, Ph.D., director, Learning Health Center for Research and Education and research assistant professor of biomedical science.
The researchers will track three parameters.
• Each week, the saliva of healthcare workers will be tested for the presence of the virus, without long waits and the discomfort of traditional methods. Saliva samples are a preferable indicator for infection than the deep nasal swabs now widely used, recent studies have shown.
• Volunteers will carry an Oura Ring, an activity and symptom tracker that measures physiological signals such as temperature, blood pressure, respiratory rate and other data. This information will be transmitted to the server, providing data to understand clinical signals for illness onset.
• Two serology tests will be conducted to identify antibodies against the virus. One test will occur during the middle of the study period and another few weeks after the study’s conclusion.
“We will follow the volunteers for three months to learn how many of them get infected, which we can see with serological and molecular tests,” Caputi said. “Are volunteers mounting an immunological response? And how strong is that response? We can identify when they get infected with saliva tests and when they have symptoms with the Oura Ring tracker. We can also learn how many were unknowingly infected but without symptoms.”
This study will provide data for a predictive algorithm, which eventually could be used in testing and prevention protocols for healthcare workplaces.