M.D. Degree Program
The Integrated Patient Focused Curriculum is based on the principle that future physicians should learn essential basic science information in the context of patient care, patient case studies, and the practice of clinical skills. We provide our students with a stimulating, supportive and collegial learning environment featuring:
- An early introduction to the patient and the community
- Continuity relationships with patients, physicians, and health care systems
- Longitudinal integrated clerkship modules in the third year
- Integrated competency assessments
- A small class size
View the College of Medicine Academic Calendar (2025-26) for Years 1, 2, 3, and 4, or check the upcoming calendar (2026-27).
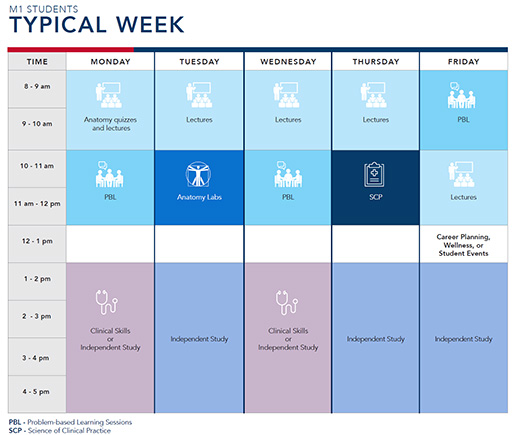
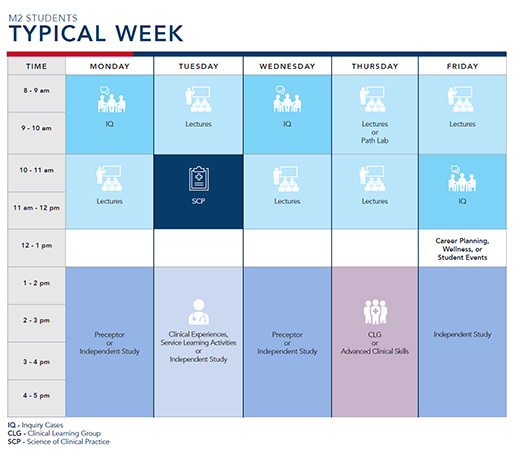
The foundational science curriculum integrates key disciplines like anatomy, physiology, pharmacology and pathology throughout the courses. Teaching methods include problem-based learning, with a balance of small group sessions and independent study, supplemented by labs, clinical correlations, simulations, and lectures focusing on core concepts rather than lists of facts.
The clinical curriculum in years 1 and 2 includes the series of four Foundations of Medicine courses. These courses are designed to provide students with an understanding of the fundamental skills and principles needed to be a compassionate, competent and professional physician. During these courses, students learn medical interviewing, physical examination, and clinical reasoning skills using a hypothesis-driven approach grounded in evidence-based medicine. Standardized and simulated patients are used to teach core and advanced clinical skills. Students also learn the concepts needed to provide effective, collaborative and patient-centered care. Starting in the spring semester of Year 1, students regularly engage in direct patient care under the supervision of physician preceptors in the community.
In our Year 3 Longitudinal Integrated Clerkships (LICs), students are placed with a group of physicians at affiliated community hospitals for an extended period, rather than completing short discipline-specific clerkships in random order at multiple sites.
At the end of Year 3, students have completed core clerkships in Medicine, Surgery, Ob/Gyn, Pediatrics, Psychiatry, and Community and Preventive Medicine and have been exposed to other medical subspecialties including anesthesiology, geriatrics, palliative care, emergency medicine, pathology, and radiology.
Throughout Year 3, students are provided with "white space time" - time set aside for students to pursue their own interests - such as clinical experiences in subspecialties, research, or community health projects. During Year 4, students have the opportunity to take a wide range of selective and elective rotations in addition to required acting internships. The Transition to Residency course throughout Year 4 prepares our students for the next phase of their education - residency.
Competencies and Objectives
The FAU Medical Education Program Goals guide the MD curriculum. The 8 Competencies* all graduates are expected to achieve are:
*This is the Physician Competency Reference Set (PCRS) endorsed by the AAMC as the common learner expectations utilized in the training of physicians and other health professionals.