By John H. Tibbetts
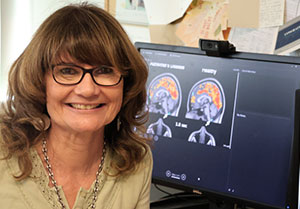
Monica Rosselli, Ph.D., wants to develop precise screening tools for Alzheimer’s disease reflective of a patient’s culture.
Early in her career, Rosselli said she realized that psychological screening tests given to Spanish speakers could be fundamentally flawed, leading to inaccurate measurements of cognitive health. These tests, intended to detect dementia and other abnormalities in the brain, were created by English speakers for English speakers and translated into Spanish. But people of different cultures and languages can misunderstand one another, even if translations are technically accurate.
Miscommunicating is about a lot more than just word definitions, she said. “Your culture influences the way you think, the way you feel, the way you behave,” said Rosselli, professor of psychology and associate chair of the department of psychology in the FAU Charles E. Schmidt College of Science.
For this work, she’s earned two grants. One from the National Institutes of Health (NIH) for $2 million and another from the National Institutes of Aging for about $2.4 million.
Multiple studies have identified significant effects of culture-associated variables — preferred language, country of origin, ethnicity, race and other factors — in how people perform on tests of cognitive health, according to Rosselli’s co-authored review in the in the journal Neurotherapeutics, in January 2022.
“When you develop a verbal or nonverbal psychological test, you are influenced by your own culture, and your culture also affects how you perform on that test,” Rosselli said. “In the 1980s, I showed for the first time that even nonverbal psychological tests were affected by the cultures of the test developer and the person being assessed. It’s almost impossible to develop a test independently from your culture. A Latin American might be diagnosed with cognitive impairment because of a test created by white Americans for white Americans. The real problem can be with the test.”
Now, Rosselli and her colleagues plan for a day when they can bring together culturally tailored assessments of dementia health with images of brain biomarkers, using state-of-the-art imaging technologies, such as an MRI. People who experience certain shrinkages in the brain — or biomarkers — could be at higher risk of Alzheimer’s disease and related diseases. Alzheimer’s patients have decreased volume in one part of the brain compared to those who are cognitively normal. “Someone who develops Alzheimer’s disease can have brain or psychological changes even before there are any manifestations in cognition,” Rosselli said.
Alzheimer’s disease is the most frequent cause of dementia in aging, and Florida is an epicenter of the Alzheimer’s epidemic in the U.S. Dementia diseases are more frequently seen in Hispanic and African-American populations compared to whites. Florida has 450,000 Alzheimer’s patients with greater than 3.2 million at-risk individuals over age 65 and large Hispanic populations.
“When you develop a verbal or nonverbal psychological test, you are influenced by your own culture, and your culture also affects how you perform on that test.”– Monica Roselli, Ph.D.
In 2020, the 1Florida Alzheimer’s Disease Research Center (ADRC), a consortium of leading research institutions that includes FAU, received a five-year $15 million NIH National Institute on Aging grant to further focus on dementia in diverse populations. The 1Florida ADRC effort focuses on why some minorities have higher rates of dementia. Researchers also aim to identify when people start to transition from normal cognition to mild cognitive and from there to dementia — and intervene with effective treatment faster.
Neuroimaging tools, including MRI exams, could help scientists learn more about potential relationships between brain tissue changes and dementia, like the size of the hippocampus, an area of the brain in the temporal lobe. “If the hippocampus volume shrinks, then patients are more at risk to develop characteristics of some dementia diseases,” Roselli said.
In a 2022 study, published in the journal Applied Neuropsychology: Adult, Rosselli’s research team compared symptoms of depression and the frequency of reported apathy in people of two ethnic groups — Hispanic Americans and European Americans. The team categorized individuals according to their cognitive condition: normal, mild impairment or dementia. The team used MRI scans to compare potential correlations between ethnic populations diagnosed with depression and apathy with brain tissue loss.
“We did find some losses in the brain volumes” among people diagnosed with depression or apathy. The tissue losses were in different prefrontal locations among Hispanics compared to non-Hispanic whites. “But we don’t yet understand what those differences mean,” she said.
