By Shavantay Minnis
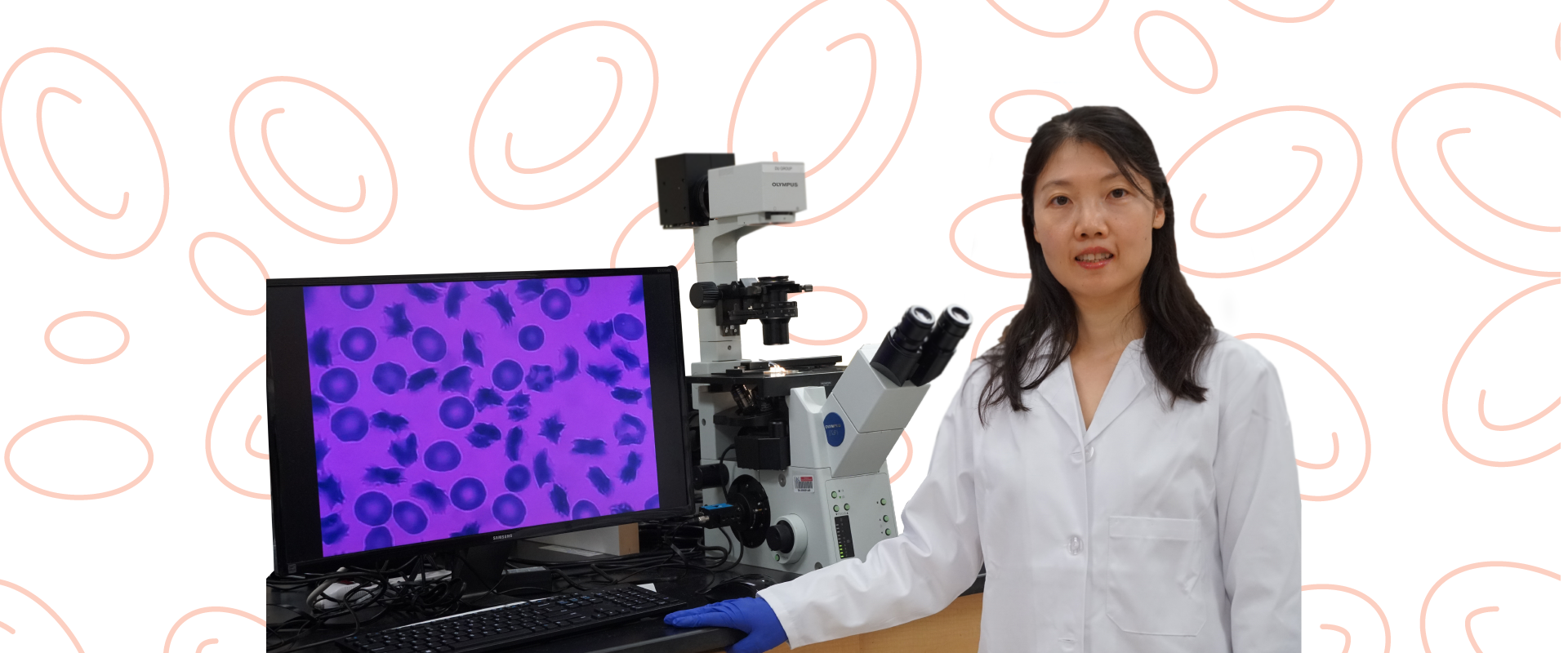
Understanding how blood cells move throughout the body could aid Sarah Du, Ph.D., in the treatment and even prevention of life-threatening diseases like sickle cell anemia and malaria.
“A single drop of blood can tell us a lot,” said Du, a mechanical engineer and associate professor in the College of Engineering and Computer Science. “From an engineering perspective, I’m very curious about the electrical and mechanical properties of the red blood cells because they tell the body how much oxygen to carry and when there is low oxygen, it creates diseases.”
To do this, Du develops tools like biosensors and microfluidic devices, or very small devices, to study red blood cells. She uses these tools to understand the properties of blood cells and get as close to a single drop of blood as possible, she said. Her devices also mimic the natural flow and function of red blood cells, using electrical signals inside the device to measure blood activity.
“Unlike traditional petri dishes that can only examine steady non-moving cells, our devices can examine the blood flow, the oxygen concentration and the cell-to-cell interaction without being concerned that the natural movement will disrupt our findings,” Du said.
When Du has a drop of blood under her devices, she can determine how much oxygen passes through, and how rigid the red blood cells become when no oxygen is available, she said.
Since red blood cells need to be extremely flexible and
easily transformed to deliver oxygen into the different organs for the body to function, Du’s devices can detect when the oxygen fails to move and how diseases like sickle cell anemia begin to progress.
“When we are looking at the difference between diseased blood cells and normal ones, the life span of the red blood cells is often shorter allowing us to know which disease to look at,” she said. “In sickle cell, for example, the lifespan is only 15 days compared to the 120 days of a normal red blood cells. This could be attributed to the much weaker mechanical properties.”
With this information, Du said one of her goals is to provide a rapid, patient-specific drug efficacy testing to improve the oxygen delivery in the blood of sickle cell patients and the other is to create a point of care at-home device for people. The latter is close
to completion.
“Once we saw how this method was more improved than using a traditional microscope and petri dish to examine the mechanical properties of red blood cells and how it relates to diseases, we wanted to see if we can bring these testing methods to the patients and to the field,” Du said. “Now with a single drop of blood, we have biosensors inside portable disposable devices with a phone application that can test red blood cells to determine and monitor the state of the disease.”
Prior to Du’s work in red blood cells and creating devices to study their mechanical properties, she studied fabrication techniques on how to make
microfluidic devices in 2011 while earning her doctorate degree at the Stevens Institute of Technology in Hoboken, N.J.
She completed her postdoctoral studies in 2014 at the Massachusetts Institute of Technology in Cambridge, Mass., where she continued learning about microfluidic devices as well as the properties of red blood cells.
Coming to FAU a month later in 2014, Du has since earned awards from the National Science Foundation for her portable smart sensor and application project and now with her methods for testing red blood cells using microfluidic devices and biosensors, she’s using it to work on other projects such as studying human organs with a chip.
Since malaria is a disease that can even target pregnant women, Du is targeting her efforts to support
the placenta.
Using a microfluidic device, she said, and a micro sensing chip, they can create a mock version that simulates the placenta barrier of a woman with
malaria disease.
“If we can capture a single cell from a placenta and examine it on a chip, we can compare how the malaria-infected blood, which can cause birth defects and sometimes death to the baby, behaves differently compared to normal blood,” Du said. “It’s a method that can contribute greatly to the health of women around the world.”